Inherited thrombophilia and cancer are both recognized risk factors for venous thromboembolism (VTE). In the general population, the risk of thrombosis is increased in patients with inherited thrombophilia, but the role of inherited thrombophilia on the risk of cancer-associated VTE remains controversial. The objective of this study was to summarize and determine whether cancer patients with inherited thrombophilia gene mutations have an increased risk of developing VTE.
We conducted a systematic literature search in Medline, EMBASE and Cochrane Central databases, as well as references of included studies from inception until September 26 th 2022. We included observational (cohort or case-control) and interventional studies comprising of human adult cancer patients who were tested for any inherited thrombophilia gene mutation. The outcome was objectively confirmed symptomatic or asymptomatic first VTE (upper or lower limbs deep vein thrombosis, pulmonary embolism, and/or splanchnic or cerebral vein thrombosis) occurring after a cancer diagnosis. Two reviewers independently screened the titles/abstracts and full texts of all potentially eligible articles. Pooled odds ratios (OR) and 95% confidence intervals (95% CI) were estimated using Mantel-Haenszel random-effects models. We used the Quality in Prognostic Studies (QUIPS) risk of bias tool to assess study risk of bias.
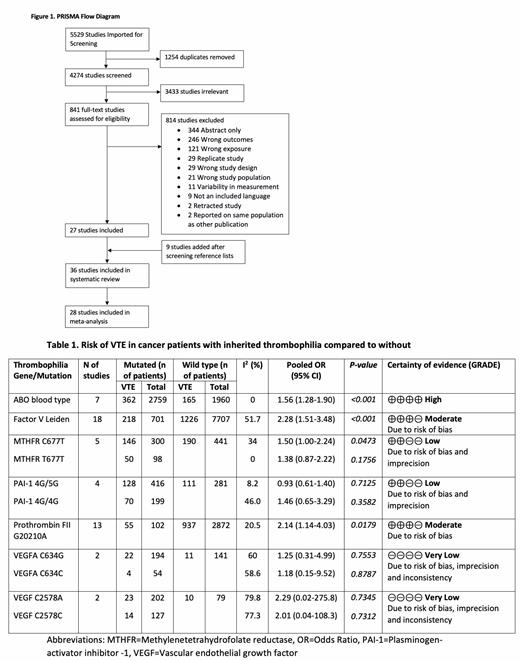
A total of 4274 studies were screened for eligibility. Thirty-six studies involving different cancer types and treatments were included in the systematic review, of which 28 studies were included in the meta-analysis (Figure 1). Among studies included in the meta-analysis, 9 studies included various cancer types while the remaining 19 studies were in selected cancer types (3 lung, 3 myeloma, 2 brain, 2 bladder, 2 breast, 2 gynecologic, 1 testicular, 1 lung or gastrointestinal, 1 pancreas, 1 colorectal and 1 breast or gastrointestinal). There were 18 cohort (11 prospective and 7 retrospective) and 10 case-control studies. The following seven inherited thrombophilia gene mutations were meta-analyzed: ABO blood type, Factor V Leiden (FVL), Methylenetrahydrofolate Reductase (MTHFR) C677T, Plasminogen-Activator Inhibitor-1 (PAI-1) 4G/5G, Prothrombin Factor II G20210A, Vascular Endothelial Growth Factor (VEGF) C634G and VEGF C2578A. In cancer patients with non-O blood types, FVL and Prothrombin Factor II G20210A mutations, the risk of VTE was significantly increased with ORs of 1.56 (95% CI: 1.28-1.90), 2.28 (95% CI: 1.51-3.48) and 2.14 (95% CI: 1.14-4.03), respectively, compared to patients with O blood and wild types (Table 1). In addition, heterozygous and homozygous MTHFR C677T were associated with ORs of 1.50 (95% CI: 1.00-2.24) and 1.38 (95% CI: 0.87-2.22), respectively (Table 1). Among those with heterozygous and homozygous PAI-1 4G/5G, VEGF C634G and VEGF C2578A, no significant increase in the odds of VTE and moderate to considerable heterogeneity were observed (Table 1). Few studies had low risk of bias, except for studies of ABO blood group, which predominantly had low risk of bias.
In conclusion, this meta-analysis provides evidence that non-O blood type, FVL, Prothrombin Factor II G20210A and heterozygous MTHFR C677T significantly increase the risk of VTE in cancer patients. However, there is moderate to high risk of bias in the currently available data, further well-designed studies are needed.
Disclosures
Wang:Leo Pharma: Research Funding; Valeo: Honoraria.